Validation of impaired Transient Receptor Potential Melastatin 3 ion channel activity in natural killer cells from Chronic Fatigue Syndrome/ Myalgic Encephalomyelitis patients.
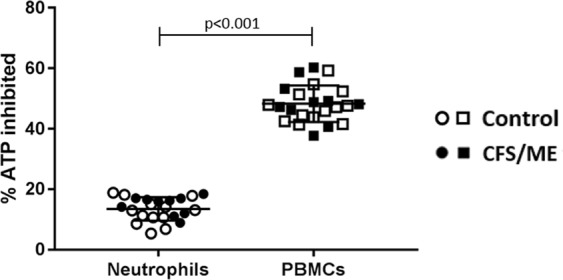
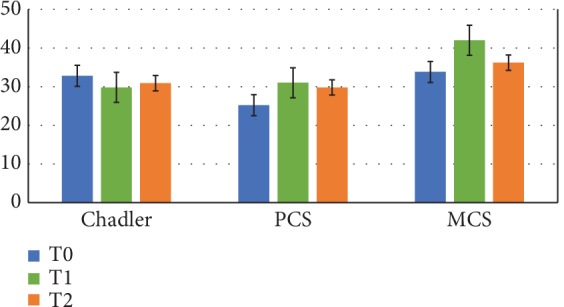
Syndrome of chronic fatigue / myalgic encephalomyelitis (CFS / ME) is a complex multifactorial disease of unknown cause with multi-system events. Although the etiology of CFS / ME remains elusive, immunological dysfunction and specifically low cytotoxic activity in natural killer (NK) cells is the result of more consistent laboratory. The transient receptor potential (TRP) superfamily … Read more